Top 9 Challenges to Mastering your Remote Patient Monitoring Operations
Remote Patient Monitoring (RPM) is growing, and it’s increasingly becoming table stakes for any type of remote care management company or program. But standing up your own RPM operations can be far more difficult than it initially appears, at least to do it efficiently at scale.
Some of the specific pains and challenges we’ve experienced and observed in doing everything internally are covered below.
Selecting your program offerings
A number of companies offer SaaS for conducting RPM programs, but they really leave it up to the practice to complete all of the operations. This is increasingly difficult in today’s staffing environment. While a few allstar practices may stand up solid programs the majority will not reach their goals, and will be disappointed before they get the momentum needed to see positive results at scale. Other RPM companies opt to offer a more full service approach, where they essentially run the program after an initial list of eligible patients is pulled. A full service option will generally result in more patients being able to access the services, but it far more operationally complex. This model can grow quickly and be highly profitable at scale but without the right design it may even be unprofitable.
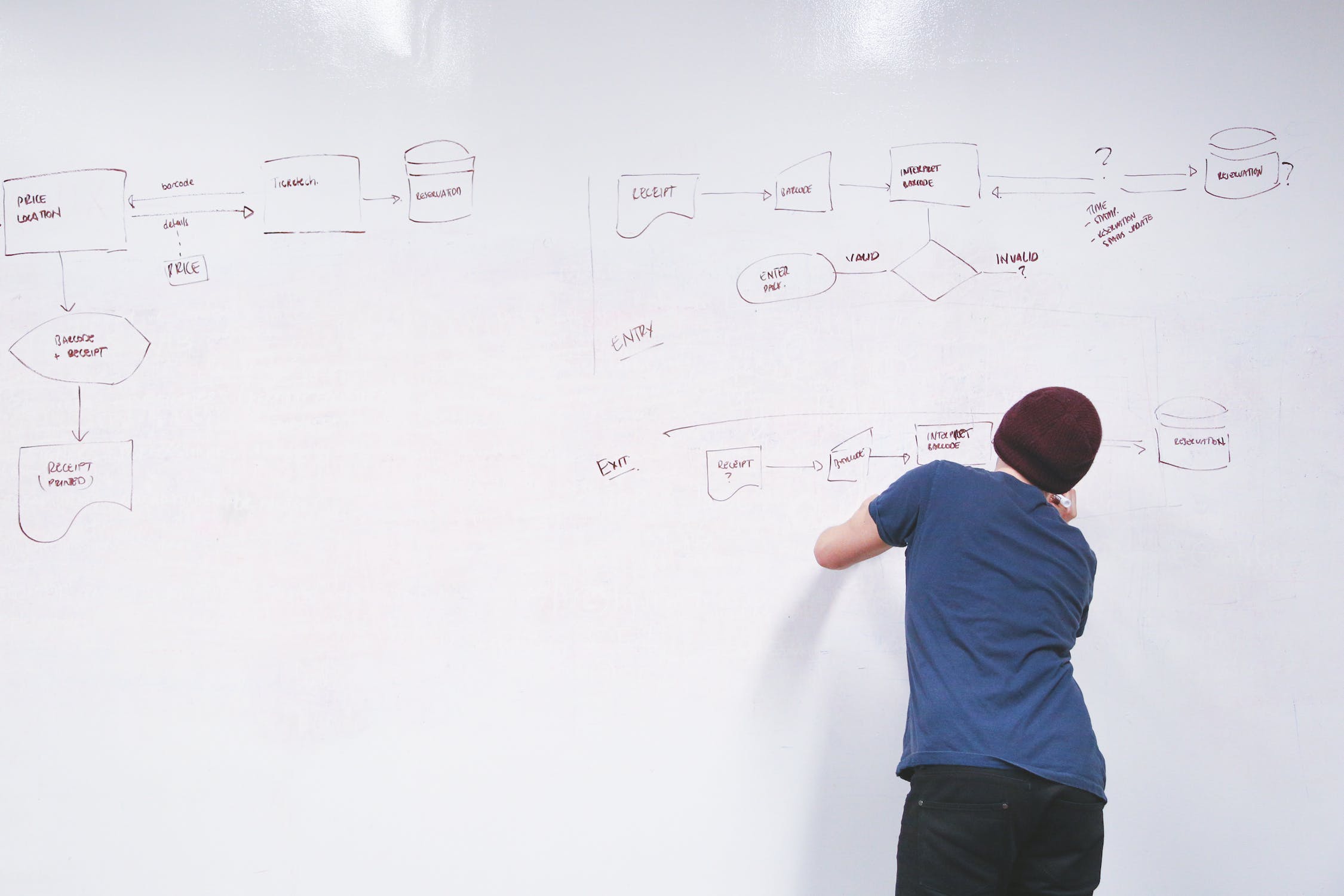
Deciding which workflows you want to support
There is a saying that if you’ve seen one medical practice you’ve seen one medical practice. There are many variations of workflows that are requested in RPM, but fortunately it’s not an infinite number. At the core, there are two major workflows that need to be considered.
The first is a workflow where the patient is given the device within the practice. These visits can be scheduled in advance and are presented as an “add-on” after the visit for qualifying patients. This is a simpler workflow in general, but it requires the practice to operationalize everything, which is not 100% in your control. Still, there are some best practices that can be shared with the practice that will increase onboarding rates with this workflow.
The second is a workflow where the patient is called, and then shipped the device via FedEx. This workflow requires some steps to be completed upfront over the phone to obtain consent, with some documentation required to ensure regulatory compliance. Appropriate follow-up after shipping is also required to ensure the maximum number of devices get set up and activated. This workflow is operationally more challenging but can result in the fastest growth when done well. It’s critical to ensure that data is captured at each step in the process and presented to the ops team so patients don’t slip through the cracks at any one step in the process.
Selecting the right devices
There are literally hundreds, if not thousands, of connected health devices out there. But integrations still take time. It can be difficult to know which ones are worth supporting without an extensive testing process. This takes time and is likely to include a reasonable amount of trial and error for somebody who has never had to do this before.
- Number of patients with the condition - the device should address a meaningful number of patients within a practice or it’s unlikely to get the time of the staff
- Clinical accuracy - the device should pass the standards for clinical accuracy on a range of patients (e.g. obese patients may create technical difficult for some weight scales or blood pressure cuffs)
- Connectivity - whether or not you are going to aim to target Bluetooth-based devices or Cellular-based devices (hint: all of the most successful RPM providers tend to use cellular-based devices).
- Regulatory compliance - devices need to meet the definition of a medical device as defined by the FDA. This generally means that they should also be registered with the FDA and have completed a 510(k).
- Reimbursement eligibility - In order to qualify for 99454, the device must transmit 16 or more days of readings out of the calendar month. Some companies have tried to get creative with their interpretation of this language, or with a temporary COVID exemption, but I’ve been told by multiple regulatory experts that that is highly risky. The safest bet is to ensure that you are selecting quality devices that people are likely to use frequently and over a long period of time.
- Cost - Cost is always a consideration and devices that cost several hundreds of dollars will rarely make sense. However, the other factors often matter more. After all, if the patient is unable to use the device then there will be no revenue. If the practice receives a large number of technical support issues or complaints then they will often kill the entire program if they are worried about damage to their reputation or clinical risks.
For more detailed info, please see our article device selection strategy (link)
Supplier and logistics management
Doing this well involves managing relationships and contracts with multiple hardware suppliers. This was something I had done before, but I found it was a relatively rare skillset to find somebody who had done that and who had also worked in the healthcare SaaS industry.
Operational software selection or design
Most companies choose to string together a few different pieces of 3rd party software. This is generally the right approach, as they wouldn’t know what to design when they are first starting out, but it can still take several months to arrive at the right combination of software packages. It’s not uncommon to start integrating and then have to take a step backwards after reaching a key blocker.
Contract design
Whether choosing to go W2 or 1099, it’s critical to design employee agreements that align incentives while also minimizing legal risk remaining competitive in the labor marketplace. There can be pros and cons to each approach.
I’ve been told confidentiality by several people who have set up or scaled RPM programs that this is an area they wish they had spent more time on initially as it’s difficult to back out of once you’ve gone down a path, especially if you’ve decided to make your entire care team full time W2 employees..
Managing efficiency with KPIs and Analytics
Professionally-run businesses generally rely on metrics to have an idea of whether or not they are reaching the targets they need to be financially successful. If you want to scale your program, it becomes critical to develop and monitor KPIs so you can ensure that members of your RPM operations team are reaching their efficiency goals. Good metrics will enable you to identify high performers so you can share their habits and tactics with the rest of the team, and to identify any process bottlenecks so you can unblock them.
The issue is that metrics, and specifically the capture of data, is often done as an afterthought. Having the right KPIs is useless if they can’t be measured effectively, and measurement is difficult to impossible when patient data is spread across different disparate systems. Here’s what I mean - many RPM companies may have different systems for checking insurance vs. making outbound calls vs. performing clinical monitoring vs. billing. If these systems aren’t connected then organizing the data will be the type of challenge that requires full time staff in itself. Compare this to a more ideal situation when patient metrics can be seamlessly viewed in a funnel-like view, as they would be in any modern marketing enterprise. This is an often overlooked area, and it’s something that our partners will have dramatically improved vs. the “many disparate systems” approach to running their operations.
Recruiting and Training
Finally, companies that decide to do this all in-house will need to build a team of people to execute it. This takes a lot of time and money to do well by the time you recruit, screen, train and manage all of these people.
Inevitably it will siphon away a substantial amount of senior executive time from other key activities like sales and fundraising. Operational issues often demand an immediate response, which can be disruptive to work or even a well-deserved vacation with your family.
What if there was a better alternative?
This may sound like a lot to take on. It’s actually even a lot more complicated than this. Fortunately there is a better alternative today than there was when we started out in RPM.
By working with Continua, you get access to an experienced team, and well-designed software, devices and processes that are already proven to scale. This minimizes your risk and may accelerate your time to scaling your RPM program by 10x, with only 1/10th the upfront cost of doing it all in house. Our offering actually goes far beyond just shipping devices - we can be your entire outsourced operations department. Contact us for a free consultation to learn more about the details.